For a booming industry built on speed and selfies, the rules of the game may be about to sharpen.
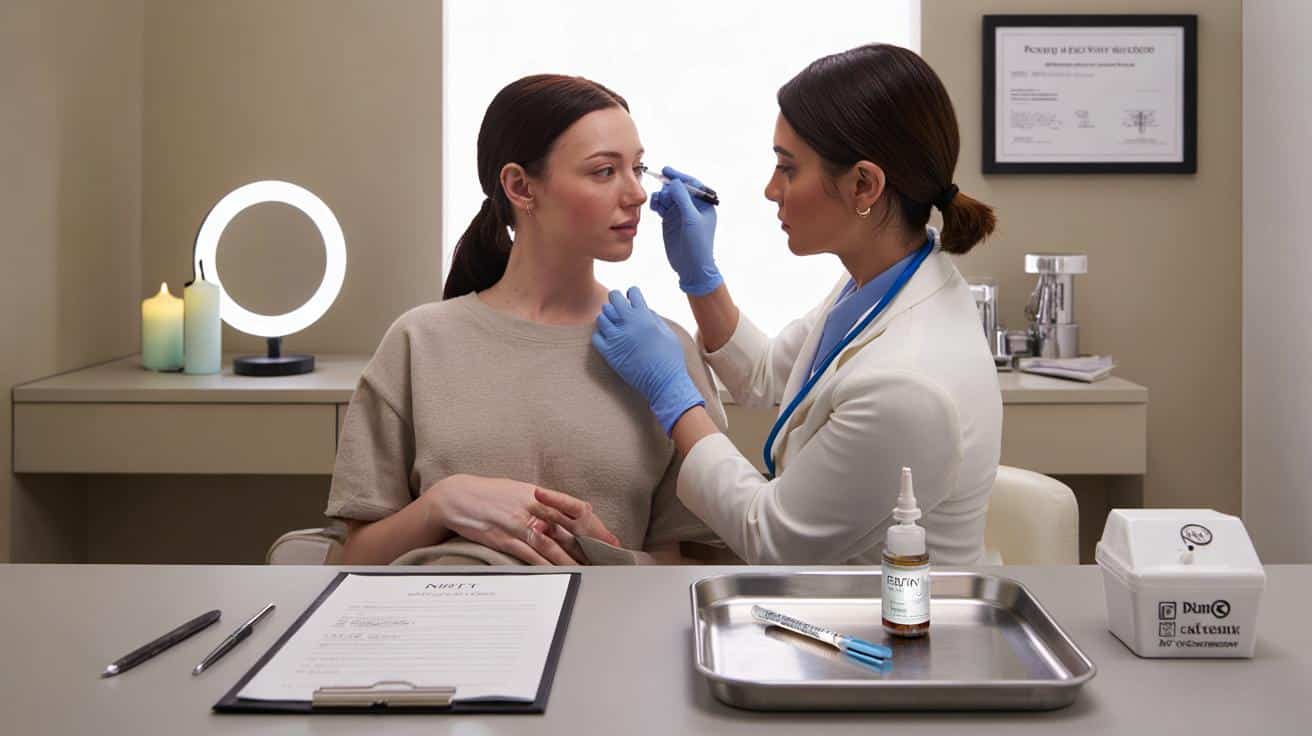
The waiting room is too perfect. Spearmint candles, latte-coloured walls, the thrum of a ring light. A woman in a parka leans in to whisper, “It’s my first time. Does it hurt?” The practitioner smiles with the well-practised ease of someone who’s answered that question all week. Outside, scooters buzz by and a bus ad promises smoother skin by Saturday. Inside, consent forms rustle. The whole scene feels at once ordinary and fragile, like a ritual we’ve collectively rehearsed without ever agreeing on the script. That script is being rewritten.
The guideline, the licence, and the quiet shift in power
Here’s the nub: Botox isn’t a beauty treatment in the eyes of the law. It’s a **prescription-only medicine**. That already means a qualified prescriber — doctor, dentist, or appropriately trained independent prescriber — must assess you before any needle goes near your face. The new NHS-aligned guidance, arriving in step with a national licensing scheme for non-surgical aesthetics, signals something bolder: higher-risk procedures like botulinum toxin injections should happen under prescriber-led oversight, with clearer competency standards and better reporting when things go wrong.
What does that look like beyond headlines? For one, the days of casual “pop-up” toxin clinics may be numbered. Industry-watchers say the Department of Health and Social Care’s licensing framework, powered by the Health and Care Act 2022, is expected to require local authority licences for providers and premises, training thresholds mapped to risk, and stronger checks on who can inject. NHS England’s safety push dovetails with that by advocating face-to-face assessment, documented informed consent, and pathways to urgent care if complications hit. It’s the administrative end of a makeover.
There’s a backdrop to this. Complaints about poor outcomes in the aesthetics sector have surged in recent years, with independent watchdogs reporting thousands of cases — many linked to non-medical settings, opaque prescribing, and patchy aftercare. Regulators already ban direct advertising of “Botox” to the public, because of its medicine status, yet social media is awash with wink-wink phrasing like “wrinkle softening”. The new guidance doesn’t reinvent the law; it clarifies, tightens, and teams up with licensing to make enforcement real. It’s a slow turn of a screw that changes leverage.
How it could change who injects, and how clinics adapt
Expect a more explicit line between “can inject” and “can prescribe and lead”. In practice, it may push clinics toward models where a prescriber conducts a proper clinical assessment — ideally in person — and either performs the injections or supervises a clearly competent injector with up-to-date training. The model already exists in well-run clinics. What’s different is the signal: a **licensing scheme** plus NHS-backed standards give councils and insurers the cover to say no to set-ups that rely on remote prescribing shortcuts or vague oversight.
We’ve all had that moment where a “friendly recommendation” blurs into a back-room top-up. That grey zone is where harm tends to hide. Save Face and other groups have long flagged cases where clients couldn’t reach their injector when swelling or ptosis kicked in at 10pm, or where a prescriber’s name appeared on paper but never met the patient. A licensing regime will make that harder. It will also reward the clinics already doing the dull, safe things well: detailed medical histories, cooling-off periods, and honest conversations about risk. Let’s be honest: nobody really does that every day.
Follow the semantics and you’ll see the shift. Remote prescribing for cosmetic Botox has been under intense scrutiny for years, and guidance steers prescribers toward **face-to-face consultation** for a proper examination before writing a script. Add local licensing checks and insurer demands, and the viable pool of injectors narrows to those who can plug into prescriber-led care with clear accountability. That doesn’t lock non-medics out entirely where law allows administering under direction, but it cranks up the required scaffolding — training, supervision, escalation plans, and auditable records — until “casual” becomes unviable.
Practical steps now: safer bookings, stronger clinics, fewer surprises
If you’re running a clinic, map your pathway against what’s coming. Start with triage: who assesses patients, how is medical suitability judged, and where is the prescriber in that picture? Build a simple paper-and-digital trail — health history, consent that’s truly informed, product batch numbers, aftercare, and a plan for complications with named responsibility. It’s not glamorous. It is the difference between a service and a system, and licensing loves systems.
For patients, a tiny script can change your outcome. Ask: who is the prescriber and when will I meet them? What’s the product, dose, and plan if something goes wrong? Where does follow-up happen and who pays for it? Clinics that welcome those questions tend to be the ones you want. The ones that wave them away often struggle when small issues snowball into swelling, bruising, or eyelid droop. *A good injector talks candidly about risk before they talk about results.*
Here’s the human side. On social media, everything looks instant, painless, and consequence-free. Real life isn’t like that, and neither is healthcare. The NHS-aligned guidance isn’t trying to kill the vibe; it’s trying to give you a clear route to help if you need it, and a standard to hold providers against. Below is a quick crib you can keep on your phone before you book.
“Good aesthetics should feel like healthcare with style, not style pretending to be healthcare.”
- Meet the prescriber: a real, named professional who assesses you, ideally in person.
- See the product: brand, batch, and storage details should be transparent.
- Know the plan: aftercare, reachable contacts, and what happens if you’re worried at 10pm.
- Ask about training: current competence in toxin injections and management of complications.
- Check insurance and premises: licensed clinic, appropriate cover, and clear complaints route.
What this means for your next appointment
You may notice small shifts: clearer consultation steps, prescribers more present, slightly slower bookings, more precise language. Clinics might retire coy euphemisms and talk frankly about botulinum toxin because the process, not the pitch, becomes the selling point. Prices could edge up where compliance costs bite; waiting rooms might calm down as pop-ups fade. For some, it will be a relief. For others, an irritation. The bigger picture is less about gatekeeping and more about accountability. Aesthetic medicine has grown up faster than its rulebook. These changes, tethered to the NHS’s safety drumbeat and a national licence, pull the industry toward healthcare norms without stripping away the artistry. The needle is still there. The scaffolding around it gets sturdier.
| Point clé | Détail | Intérêt pour le lecteur |
|---|---|---|
| Prescription-only status | Botulinum toxin is a medicine requiring a qualified prescriber’s assessment | Know who must see you before any injection |
| Licensing scheme | Government plan for local licences, training thresholds, and premises checks | Spot clinics that meet rising safety expectations |
| NHS-aligned standards | Push for prescriber-led care, robust consent, and complication pathways | Choose providers that treat aesthetics like healthcare |
FAQ :
- What exactly is changing with Botox rules?The law already says botulinum toxin needs a prescriber and can’t be advertised to the public. The shift is a new licensing regime plus NHS-backed safety guidance that tighten oversight, make standards clearer, and make enforcement easier.
- Will non-medics be banned from injecting?Not automatically. Where law allows, they may still administer under a prescriber’s direction. The bar will rise: verified training, prescriber-led assessment, clear records, and safe premises will be harder to sidestep.
- Do I have to see the prescriber in person?Guidance steers toward a proper clinical assessment by the prescriber, ideally face-to-face for cosmetic use. Remote shortcuts are under scrutiny, and insurers and councils may expect in-person reviews for higher-risk procedures.
- Can clinics advertise “Botox” deals?No. UK rules prohibit advertising prescription-only medicines to the public. That’s why you see phrases like “wrinkle relaxing”. Any provider pushing “Botox” to consumers is ignoring the ad rulebook.
- What should I ask before booking?Who is the prescriber and when do I meet them? What’s the product and dose? What’s the plan if I’m worried later? Is the clinic licensed and insured? A good clinic will answer plainly — and put it in writing.