Researchers in the UK and Scandinavia say the disease follows a crucial early switch that shapes whether modern therapies work. The insight opens the door to earlier, smarter interventions, including vaccines tailored to the tumour’s behaviour.
The early tipping point
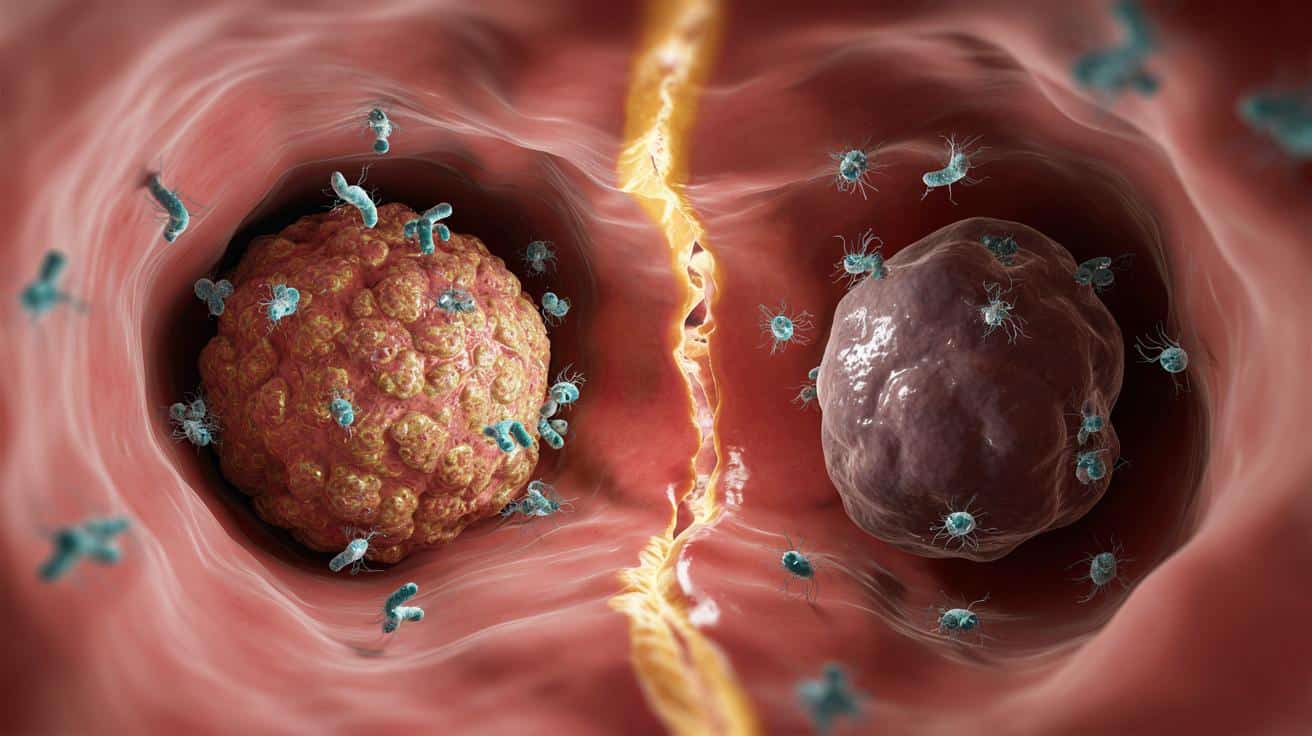
Scientists have traced a decisive “big bang” moment in bowel cancer. It happens when tumour cells first slip past the body’s immune defences. At that point, the cancer alters or disables genes that help the immune system recognise threats. Once this immune escape takes hold, the tumour’s relationship with immunity appears to settle into a stable pattern as it grows.
Teams at the Institute of Cancer Research in London and partners examined bowel cancer cells from 29 people. They tracked the genetic changes tied to immune evasion and how these changes sculpt the tumour’s visibility to T cells. Their results suggest that many tumours don’t keep evolving new ways to dodge immunity. Instead, they set that trajectory early, then amplify it as the disease progresses.
Early immune escape looks like the moment that fixes how a bowel tumour and the immune system will face off for the rest of the disease.
Why this matters for you
Bowel cancer remains the UK’s fourth most common cancer, with about 44,000 people diagnosed each year. Immunotherapy offers real benefit for a minority of patients, but only around 15% of cases respond well. If doctors can identify the immune escape pattern early and treat quickly, they could raise that number and deliver benefit sooner.
Timing could be everything. If the tumour’s immune behaviour locks in early, then targeting that behaviour before it hardens might yield stronger, longer-lasting responses. That logic helps explain why vaccines and immunotherapy combinations sit high on research agendas.
What the researchers found
The study mapped when and how bowel tumours hide. Immune escape commonly involved disrupting the machinery that flags abnormal proteins to the immune system. With those signals dimmed, T cells miss their cue. The researchers saw limited change in this immune signature later on, which implies the cancer’s strategy forms near the start.
Think of it as two diverging paths: one where the tumour stays visible and vulnerable, another where it goes dark and hard to hit. The fork appears early.
Key numbers at a glance
- 44,000: approximate annual bowel cancer diagnoses in the UK.
- 15%: proportion of bowel cancers that currently respond well to immunotherapy.
- 29: number of patients whose tumour cells were analysed in this study.
From theory to the clinic
These findings support a push for earlier biological profiling of tumours. If clinicians can measure immune escape signatures at diagnosis, they can sort patients into clearer treatment tracks. Some could head straight to immunotherapy. Others might need vaccines that retrain immune cells, or drug combinations that restore tumour visibility before immunotherapy begins.
Personalised cancer vaccines seek to prime the immune system against the tumour’s unique mutations. If a tumour has already turned off key signals, a vaccine might still work if given early and paired with agents that revive immune recognition. That is why researchers speak of a window of opportunity soon after diagnosis.
Before and after the immune escape
| Feature | Before escape | After escape |
|---|---|---|
| Immune visibility | Higher; T cells can recognise more tumour signals | Lower; disrupted signalling reduces recognition |
| Therapy sensitivity | Potentially better for immunotherapy | Reduced without combination strategies |
| Tumour evolution | Immune behaviour still malleable | Immune behaviour appears relatively fixed |
What this means for treatment choices
Doctors could soon use immune escape markers to triage options. Some patients might get surgery plus a vaccine course. Others might receive immunotherapy first if the tumour still shows clear immune targets. Where immune visibility looks low, clinicians could add drugs that restore antigen presentation or lift immune suppression in the tumour microenvironment.
Such tailoring promises sharper use of resources and fewer ineffective cycles of therapy. It also gives researchers a clean target for new drug development: keep tumours visible, or turn visibility back on.
Limits and next steps
The current work analysed tumours from 29 patients, so larger studies are needed. Researchers still need biomarker tests that reliably detect early immune escape in routine samples. Clinical trials must also test whether treating earlier on the basis of these signals boosts survival and quality of life.
Backers such as Cancer Research UK and the Wellcome Trust say this molecular map can speed up those trials. The Institute of Cancer Research team emphasises that early intervention will matter most if clinicians can spot the escape pattern at or near diagnosis.
How you can act today
Screening helps more than any single drug when it finds bowel cancer early. The NHS offers home stool tests to eligible adults through national screening programmes. People with bowel symptoms should speak to a GP without delay. Early diagnosis increases the chance of catching a tumour before immune escape sets a difficult course.
- Be alert to persistent changes in bowel habit, bleeding, unexplained weight loss, or ongoing abdominal discomfort.
- Know your family history and tell your doctor if relatives had bowel cancer or advanced polyps.
- If offered a home stool test, complete it promptly; it can pick up blood you cannot see.
Terms to know and a practical example
Immune escape: this is when a tumour stops displaying enough warning flags for immune cells to notice. Many bowel tumours alter genes that present antigens, which are fragments of abnormal proteins. Without clear antigens, immune cells cannot lock on to the cancer.
Imagine a patient whose tumour still displays antigens at diagnosis. A test flags strong immune visibility. The team chooses immunotherapy alongside surgery. Another patient shows weak visibility. The team starts with a short course of a drug that restores antigen presentation, then adds a personalised vaccine, and keeps surgery on schedule. The biology, not just the tumour’s size, shapes the plan.
Risks, benefits, and what to ask
- Potential benefit: earlier, targeted use of immunotherapy and vaccines for those most likely to respond.
- Potential risk: overtreatment if tests misclassify immune behaviour; better biomarkers can reduce this.
- What to ask: whether your pathology report includes immune-related markers and whether a trial suits your case.